Rapid On-site Evaluation: A Radiology Perspective
Sarah Martyn Consultant Sonographer Royal Cornwall Hospitals NHS Trust
In this months BAC blog: Sarah discusses ROSE from a radiology perspective

Sarah Martyn Consultant Sonographer Royal Cornwall Hospitals NHS Trust
The Royal Cornwall Hospital’s (RCHT)radiology department performs approximately 80-90 head and neck ultrasound scans each week on patients referred by their GP, oncologist, max fax, oral surgery, or ENT department. These scans are performed by sonographers or radiologists within various clinical settings; from one stop neck lump clinics to peripheral hospital sites around the county. Patients often present with a lump or swelling in the head/neck region. Some have known cancers with a query of recurrence, and for others the scan is the 1st point of contact following on from referral for the scan.
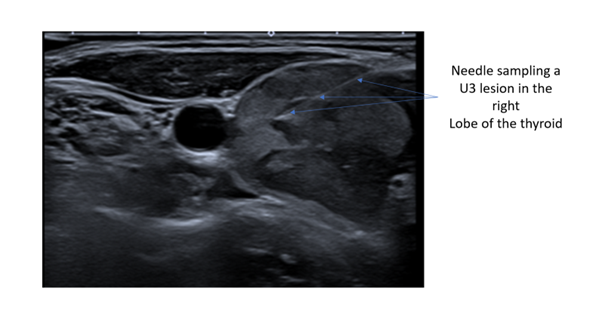
Performing fine needle aspiration (FNA) on a potential malignancy that we see during the ultrasound scan is the safest, cheapest, least invasive, and usually quickest way to obtain cellular material for diagnosis. FNA often negates the need to perform a core biopsy, thereby reducing the increased risk that comes with using a larger biopsy needle which include bleeding, infection, or pneumothorax (if lump is low down in the neck), and unlike a core biopsy, no anaesthetic is required. This reduces the potential for adverse reactions. FNA is easier than core biopsy to access small, challenging nodules that lie close to various major blood vessels within the neck. It is also less invasive for the patient.
A limitation to FNA is that samples can be insufficient at times, or not enough material is collected to carry out the various molecular tests that may be required to make a full and accurate diagnosis.
Rapid on-site evaluation (ROSE) is proven to increase adequacy rates on the first visit, negating the requirement for repeated further scans and FNAs. ROSE involves having a biomedical scientist or pathologist on site during specimen collection to analyse the material at time of collection. They are then able to advise if an adequate and sufficient sample has been performed before the patient leaves the room. The operator is directed by the scientist /pathologist and further FNA passes may be required before enough material is obtained.
The Royal College of Pathologists stated in 2019 that the most cost-efficient method of providing such a laboratory service to head and neck clinics with no compromise to quality is to have trained biomedical scientists attend these clinics to provide on-site assistance and specimen adequacy assessment (ROSE).
In 2020, the British Association of Head and Neck Oncologists advised all ultrasound guided fine needle aspiration cytology should be subject to ROSE. They state that this should be the standard of care. From a radiology perspective, as ROSE has become more available at RCHT, we have seen a larger reduction of inadequate samples and therefore patients having to return for repeat procedures.
Collaborative working
It is great to be able to work closely with the cytology department. Good communication between radiology and cytology when in the room with the patient is a key component to successful sampling and diagnosis. It can be challenging to discuss potential pathology when in front of the patient as the patient may not know yet what they are facing, and so key words are often used to establish what pathology we are dealing with and whether we need to go on and perform a core biopsy (required when suspecting some types of lymphoma). Having immediate feedback is extremely useful for correlating the radiology findings to the pathological findings.
Training
Having a biomedical scientist or pathologist in the room at time of FNA ensures optimum slide preparation. There is quite an art to spreading the sample slides correctly. Inadequate slide preparation can lead to non-diagnostic samples, delaying diagnosis and treatment. Ensuring a scientist prepares the slides adequately allows the operator to concentrate more on their other roles; scanning, performing the FNA/biopsy, filling out paperwork and making the patient feel as comfortable as possible.
Whilst training to become an independent radiology practitioner, it is so beneficial to have ROSE in the clinic setting when performing FNAs, the immediate feedback gives opportunity for the trainee to think more about the site they are sampling from and if inadequate, further attempts can be made in a different area of the lesion (less necrotic or cystic area), or indeed a different site can be attempted. ROSE enables the operator to analyse their technique, change their needle approach if necessary, and size/length of needle used. The immediate feedback is invaluable for this and helps the trainee to increase their confidence when performing FNAs. Correlating the radiology findings to the pathological findings helps the operator to understand the ultrasound characteristics of a certain pathology which is also invaluable when training.
Time
Having ROSE input can mean that extra time is required for each appointment. Once each pass is obtained a few minutes is required to prepare the slides, look under the microscope, and decide if enough cells are present to diagnose. If this procedure must be repeated (sometimes 2, 3 or more times) then this impacts on the clinical time slot given for each patient. Failure of an adequate sample after 3/4 attempts can mean the operator needs to go on and perform a core biopsy. In the standard 20-minute time slot given, the clinic has potential to overrun!
Mini MDT
Feedback from ROSE at time of FNA, enables the operator to decide if cross sectional imaging will be required and can arrange for this in advance. In turn, the patient has the potential to have all scans required performed and a diagnosis/treatment much more quickly than would conventionally occur if the service did not have ROSE alongside it.
ROSE is an invaluable service which massively benefits the radiology team and more importantly the patients. Knowing that we have sufficient material to diagnose on the first appointment significantly reduces the wait for treatment which provides some reassurance and comfort to patients in what is otherwise a very worrying time for them.
